Treatment Options For Budd-Chiari Syndrome
Shunting
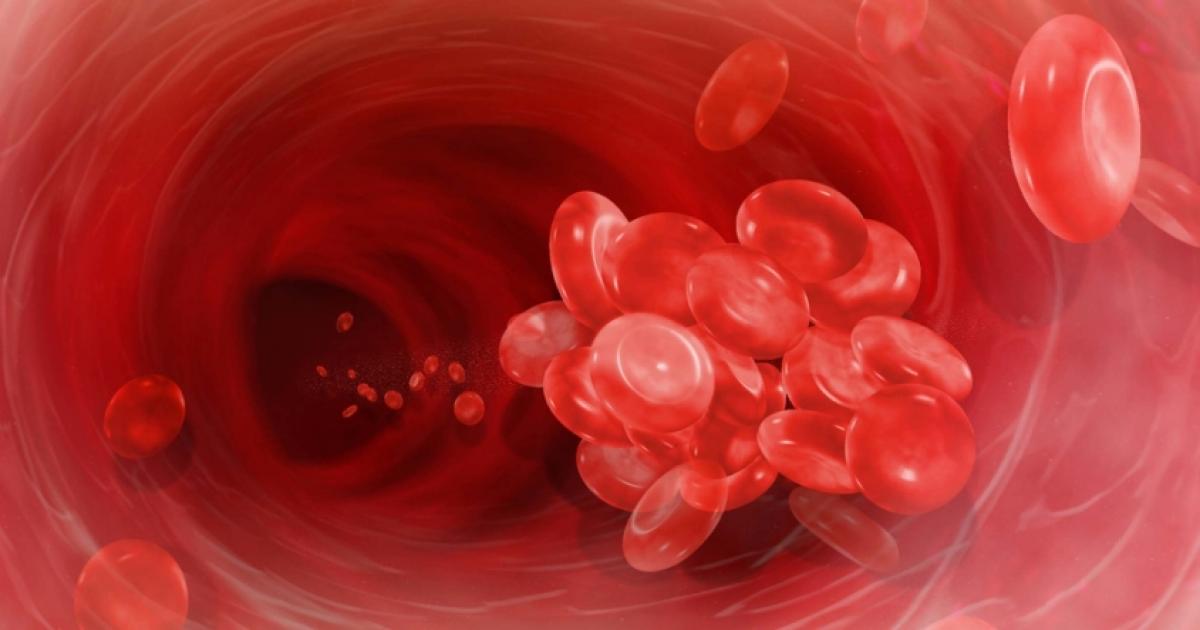
If procedures to open and widen blood vessels are unsuccessful, doctors may recommend shunting. Formally known as transjugular intrahepatic portal-systemic shunting, this operation bypasses the liver and creates a new path for blood flow. Pressure in the portal vein, which can be very high in patients with Budd-Chiari syndrome, is also reduced with this technique, which is performed with local anesthesia. Surgeons numb the neck area and insert a catheter into the jugular vein of the neck. The catheter carries a cutting needle on its tip. Doctors advance the catheter until they reach the hepatic vein, a major vessel in the liver. The needle on the end of the catheter forms a bridge between the hepatic vein and another vein in the liver, creating the new pathway for blood flow. To keep the pathway open, doctors also insert a stent at the site. After the procedure, patients will need monitoring to determine if the shunt has become blocked. This is a possible complication of the procedure, and patients who are prone to blood clots are at an increased risk for shunt blockage. The operation may also increase the likelihood of developing hepatic encephalopathy, a deterioration in brain function that occurs due to liver malfunction.
Learn more about treating Budd-Chiari syndrome effectively now.