What Are Common Herniated Disc Symptoms?
Discs are the shock absorbing elements of the spine, and are found between each vertebra in three areas of the spine: the neck (cervical region), midback (thoracic area), and lower back (lumbar spine). These three regions give our spine mobility. Spinal discs are a cartilaginous ring surrounding an inner jelly. A herniated disc refers to an injury that causes the jelly to squeeze out of place. Disc herniations are most common in individuals from thirty to fifty years old. Youth helps preserve disc function early in life, while age tends to degenerate the discs enough that herniation is unlikely. Get to know the common symptoms of a herniated disc now.
Numbness Or Tingling
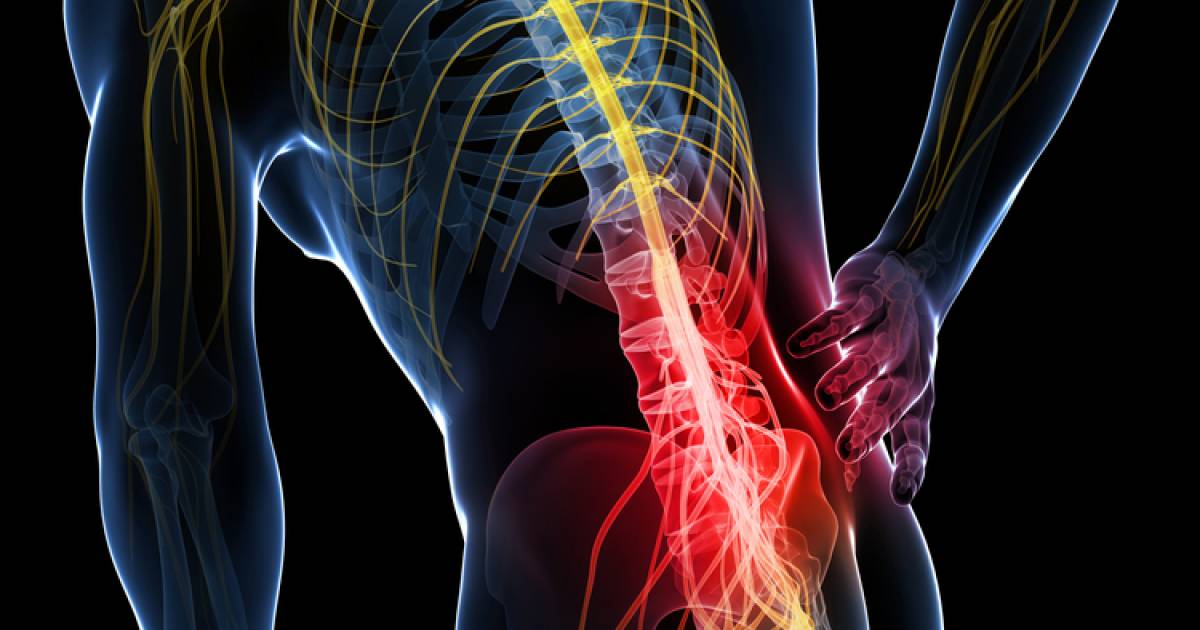
Herniated discs come with a myriad of symptoms. Some herniations are completely painless while others cause severe dysfunction. Numbness or tingling (neuralgias) is a common symptom of spinal disc herniations, They can occur together or separate. When the herniated disc is seen in the cervical area, these neuralgias tend to occur in the arms, hands, and fingers. The sensation is often described as a 'falling asleep' or 'pins and needles' sensation. Herniated discs in the lumbar spine impact the legs. Neuralgias occur because there is pressure on the area of the nerve that carries sensation. It is very individualized. A herniated disc in the same area could create numbness in the toe of one individual while causing tingling and pain in the thigh of another.
Learn more about the common signs of a herniated disc now.
Muscle Weakness

When a spinal disc herniates, the jelly that squeezes out can apply pressure to a nerve. Spinal nerves carry pain and other sensations as well as motor function. Direct pressure on the aspect of the nerve that carries motor ability will cause muscle weakness. Herniated discs tend to create weakness in the extremities, and at times the muscle weakness is profound enough to cause visible muscle atrophy. It is not uncommon, however, for a patient to be completely unaware of the muscle weakness. During an examination, a physician is able to isolate individual muscle actions to detect the problem early. It is also possible to have muscle weakness without any other symptom such as pain, numbness, or tingling. Weakness from a herniated disc may be a very serious complication and should always be evaluated by a healthcare professional.
Continue reading to reveal the next symptom of a herniated disc now.
Pain With Certain Movements

The human spine allows for extensive mobility and each individualized level of the spine consists of two adjacent vertebrae and the intervertebral disc between them. When analyzed, the vast majority of movements occur through the spinal disc with the vertebrae providing stability. This means every movement that doesn't hold the area of a disc herniation completely still causes stress to the injured disc. Just like any injured tissue, herniated discs can generate pain or discomfort. However, not all actions impact the injury in the same fashion, making it common to experience pain with certain movements only. Which movements will those be? This is determined by the area involved, the severity of the injury, as well as the overall health of the other structures in the spine.
Get the details on more herniated disc symptoms now.
Worsened Pain At Night

There is nothing more frustrating than not being able to sleep through the night. When someone struggles with pain, mobility loss, weakness, numbness, or tingling throughout the day, surely exhaustion takes over and their herniated disc is no longer problematic, right? Not always. Disc herniations may generate worsened pain at night. One of the theories as to why this occurs is known as The Gate Control Theory of Pain, which is based upon the premise that nerves can only carry a finite amount of information. During the day, the brain processes all sorts of data, meaning it is distracted from the pain. At night, the pain may intensify when these distractions are eliminated. Another theory claims pain may also be worsened at night because all day long body weight is pressing on the herniated disc, increasing its workload. With hours of repetition, this fatigues the injured disc, intensifying the pain during the night.
Get familiar with another symptom of a herniated disc now.
Location Of Pain

Herniated discs are common, yet the location of their pain is highly varied. The region of pain may be the site of the herniation, such as the neck or lower back. However, due to the potential of herniated discs to impact spinal nerves, the pain may occur at a distal site, typically an arm or leg. The nerves that exit the spine create a roadmap of sensation to the entire body. These dermatomes are predictable patterns of pain location that may actually be helpful. Physicians are trained to utilize the information such as the location of pain to help analyze which disc is impacting a certain nerve. Identification clinically is then matched up with what is visualized on radiographic image, specifically MRI or CT scans. All of these symptoms, or pieces of the disc herniation puzzle, help tailor proper treatment to the individual, thus maximizing recovery.
Continue reading to reveal more common herniated disc symptoms now.
Muscle Spasms

Patients with a herniated disc often experience muscle spasms. These happen when the muscles near the disc involuntarily contract, and they can cause moderate to severe pain. In some cases, muscle spasms could indicate a herniated disc has ruptured, and patients should have a prompt medical assessment if they experience increasing pain from spasms or if the spasms become more frequent. Patients with this symptom may have trouble exercising, and general movement during daily activities may be painful. To ease spasms and keep the patient comfortable, doctors generally recommend the use of pain relievers and muscle relaxants. Muscle relaxants may be given by injection, and patients should be aware of potential side effects such as dizziness and sleepiness. Physical therapy can strengthen muscles, and it may reduce spasms. Doctors generally recommend physical therapy if a patient's symptoms have not improved after six weeks of conservative treatment.
Discover additional warning signs of a herniated disc now.
Bowel Incontinence

Bowel incontinence is a severe complication that may develop with herniated discs, and it is also a potential sign of a serious condition known as cauda equina syndrome. This condition causes the compression of the cauda equina (the nerve roots of the spinal cord). Patients who have herniated discs and bowel incontinence are advised to seek emergency medical attention; emergency surgery may be necessary to prevent paralysis or permanent weakness. In conjunction with bowel incontinence, individuals with complications related to herniated discs may also experience bladder incontinence, and they may become entirely unable to urinate, even with a full bladder. Getting early treatment for a herniated disc can reduce a patient's risk of developing bowel issues and other severe complications.
Read more about indicators of a herniated disc now.
Neck Stiffness

Individuals who have a herniated disc in the upper back or neck may experience neck stiffness. This symptom makes it difficult to sleep and perform daily activities, and the stiffness may be worse in the mornings. Doctors can evaluate the severity of neck stiffness by asking the patient to perform certain movements, including touching their chin to their chest and touching their ear to their shoulder. Stiffness is often accompanied by pain that may vary in severity. To increase the range of motion in the neck and reduce pain, the patient may be advised to have physical therapy, and pain relievers are usually prescribed. If the pain is mild, patients might want to take an over-the-counter pain reliever such as ibuprofen or acetaminophen. For moderate to severe pain, doctors can prescribe a short course of narcotic medicines like codeine to manage the pain more effectively. Some patients find anticonvulsants can help reduce the nerve pain that may occur with neck symptoms. In addition to medications, applying ice or heat to the neck can help to temporarily ease movement and reduce pain. Patients may apply whichever is more soothing to them, and it is recommended that either ice or heat be applied in increments of twenty to thirty minutes at a time. The ice pack or heating pad should always be covered with a towel to prevent direct contact with skin. Gentle massage can also alleviate pain, and a physical therapist or medical massage therapist will instruct the patient in the most effective massage techniques for treating their pain.
Learn more about herniated disc symptoms now.
Worsened Pain After Sneezing or Coughing

The majority of patients with herniated discs will have worsened pain after sneezing or coughing. Both coughing and sneezing place stress on the back, and this can lead to increased pain. To reduce this risk, it is important for individuals with herniated discs to also take care of their general health and take steps to prevent coughs and sneezes. For example, patients might wish to take decongestants if they have an upper respiratory infection that causes coughing, and nasal sprays may help reduce the amount of sneezing a patient experiences due to seasonal allergies. If a patient notices a sudden, severe pain that does not subside after a cough or sneeze, they may wish to be examined at an urgent care facility or schedule a same-day appointment with a doctor. Any sudden, severe pain that does not subside could mean the disc has ruptured or additional damage has occurred, and this may need to be corrected promptly.
Keep reading to learn more about spotting a herniated disc now.
Sciatica

Herniated discs frequently result in pain that radiates down the sciatic nerve, a major nerve that extends from the lower back and into the legs. This type of pain is known as sciatica, and it normally only affects one side of the patient's body. To diagnose sciatica, doctors will check the patient's muscle strength, and the reflexes and sensation will also be examined. The patient may be asked to lie on their back and lift each leg individually, and the clinician might ask the patient to walk on their toes or heels. During these movements, the doctor will check the patient for any signs of pain. While most cases of sciatica resolve on their own within a few weeks, surgical interventions are available to help patients who have experienced symptoms for a prolonged period. Anti-inflammatory medicines, anticonvulsants, narcotics, and muscle relaxants may all be recommended to relieve pain. In addition, physical therapy and steroid injections might be beneficial for some individuals.